Key Takeaways
- Stop calling healthcare "broken." It's working as designed on an obsolete, 100-year-old blueprint. AI is the imperative to architect its replacement.
- Your zip code is a pre-existing condition. AI is the only tool powerful enough to smash the geographic silos that create deadly care disparities for rural populations.
- AI is the universal translator for healthcare's data chaos. It's the key to finally unlocking interoperability and turning fragmented data into life-saving insights.
- De-institutionalize your experts. AI allows you to project the expertise of your best specialists from your urban centers into every community, anytime.
- The future of health is predictive, not reactive. Use AI to shift from an expensive "break-fix" model to a proactive system of continuous monitoring and early intervention.
Let's stop repeating the tired mantra that our healthcare system is "broken." It is not. It is, in fact, a perfectly designed machine, ruthlessly executing a set of principles from a bygone era. But this is a dangerous misdiagnosis. We've decried its staggering costs, its infuriating inefficiencies and its tragic inequities. It is an industrial-age fortress built to deliver reactive, episodic care within its own walls.
The problem is, that world no longer exists. And for Americans in rural communities, this obsolete design is a death sentence, where their zip code is a more potent predictor of cancer survival than their genetic code. The answer isn't to patch this failing system. It's time to architect its successor, and AI is the indispensable tool for the revolution.
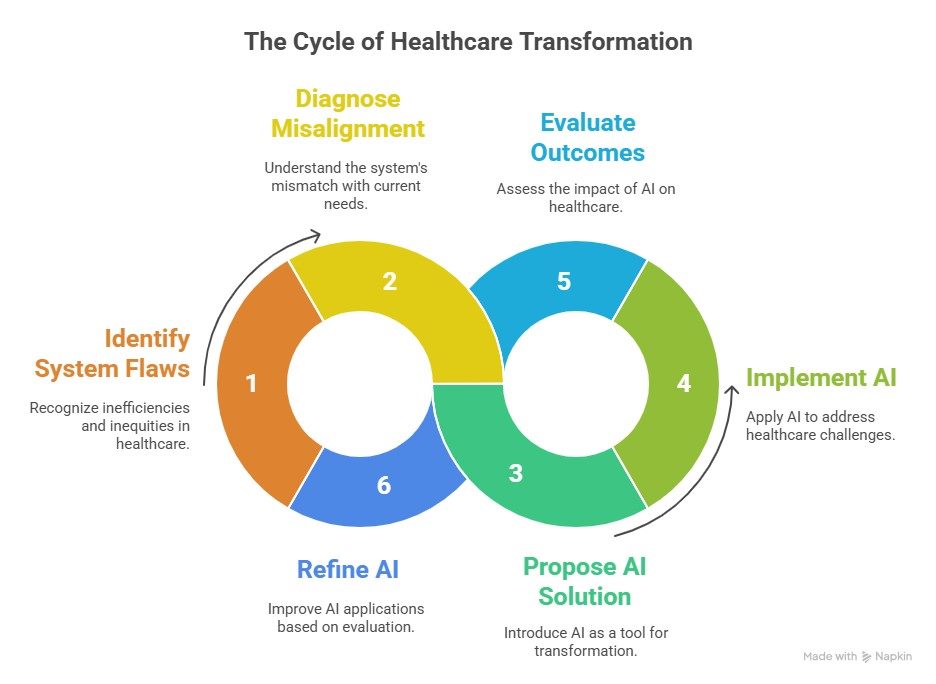
We are trying to solve 21st-century problems of chronic disease and demographic shifts with a 20th-century industrial logic. The result is a system that creates massive financial losses and, far more damningly, profound care disparities. This is not a system in need of repair; it is a system in need of radical reinvention. And the catalyst for this revolution, the tool that finally gives us the power to smash the old orthodoxies, is artificial intelligence.
Geography: Healthcare's Deadliest Border
Nowhere is the failure of our current design more apparent than in rural America. Nearly 20% of the population lives in these communities. Yet, they face a cruel paradox: higher rates of cancer and other serious diseases, but severely limited access to the specialized care needed to fight them.
For a patient in a small town diagnosed with a complex oncology case, the journey to a specialist at a major cancer center can mean hours of travel, lost wages and immense family strain, barriers that often lead to delayed or forgone care.
This isn't a bug in the system; it's a core feature of its centralized, fortress-like design. Your access to world-class care is dictated by your proximity to a handful of elite institutions. Your zip code has become a pre-existing condition, and for too many, it's a fatal one.
Related Article: 7 Ways AI Is Delivering Real-World Change in Healthcare
AI as the Universal Translator for Healthcare's Tower of Babel
At the heart of this geographic and institutional fragmentation is a problem we've talked about for years with little progress: the scandalous lack of interoperability.
Our EMRs, payer systems and provider networks are a digital Tower of Babel, each speaking its own proprietary language, incapable of meaningful communication. This isn't just an IT headache; it's a direct threat to patient safety and a massive source of financial waste.
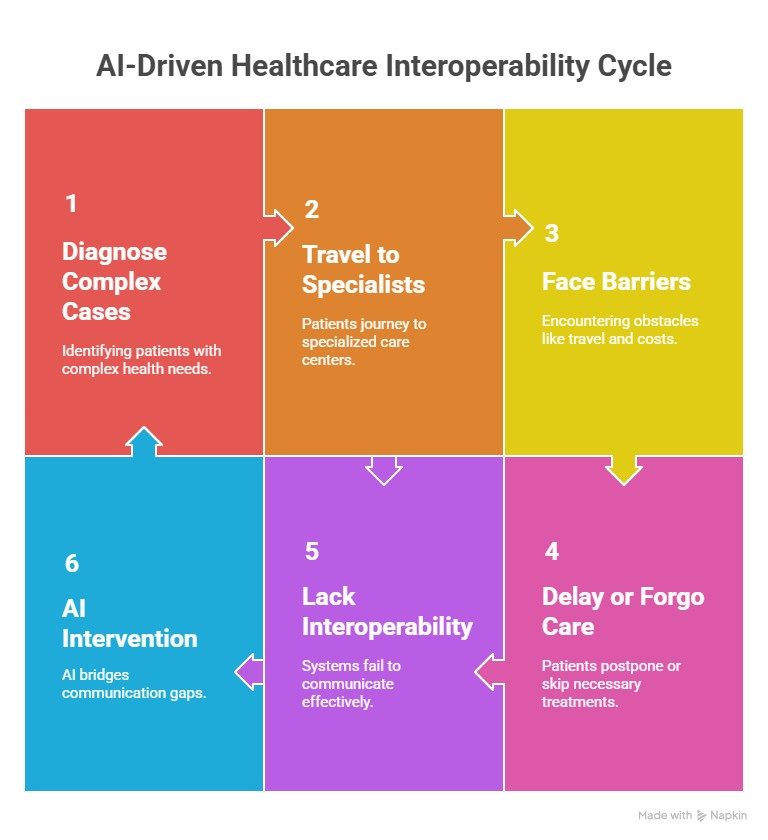
This is where AI makes its first, decisive intervention. It can act as the universal translator we've desperately needed.
- Real-World Impact: AI algorithms can now ingest, clean and structure the chaotic, unstructured data from disparate EMRs, lab reports and payer claims in real-time. This doesn't just create a unified patient record; it generates immediate, life-saving insights that were previously buried in digital noise.
De-Institutionalizing Expertise: AI's Wrecking Ball for the Fortress Walls
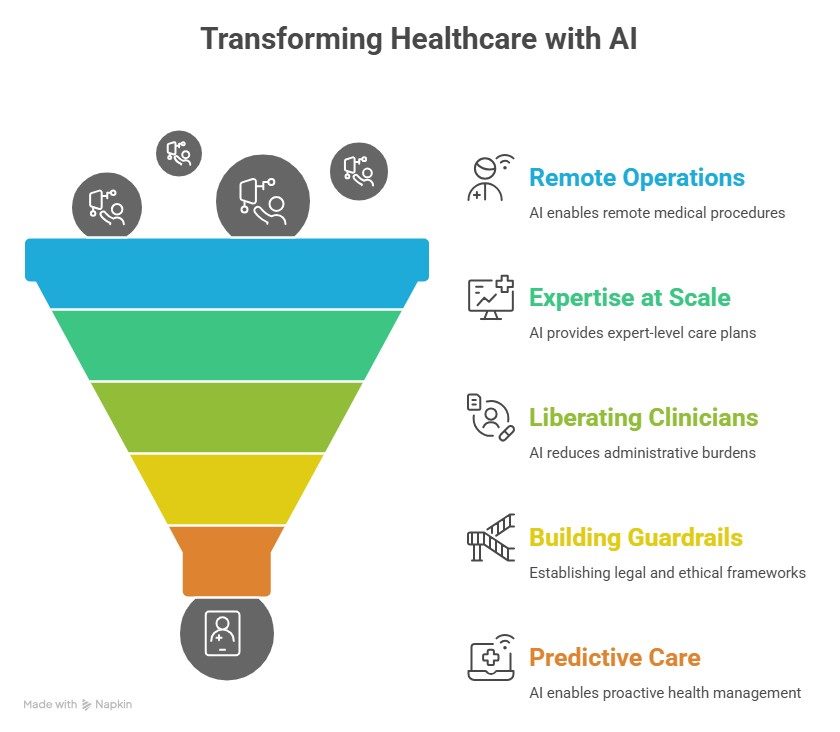
With the data problem solved, AI can then begin to dismantle the physical walls of the healthcare fortress, democratizing access to elite expertise regardless of geography.
- Remote Operations: We are now seeing AI enable the remote operation of complex medical equipment. A highly skilled technician in Boston can oversee a CT or MRI scan being performed in rural Montana, guiding the on-site staff and ensuring quality, eliminating the need for a full-time, on-site specialist.
- Expertise at Scale: An AI model, trained on millions of previous oncology cases from centers like Memorial Sloan Kettering, can generate a world-class radiation therapy plan for a patient in a community hospital, a plan that is then reviewed and approved by the local oncologist. The AI isn't replacing the doctor; it's giving them the distilled expertise of thousands of their peers as a powerful decision-support tool.
- Liberating Clinicians: AI-powered scribes and documentation tools can automate the crushing administrative burden that consumes so much of a clinician's time, freeing them to focus on complex patient care, whether in person or via telehealth.
Related Article: 5 Levels of AI in Healthcare: From Chatbots to Scaled Innovation
The Hard Work Ahead: Building the Guardrails for a New Era
This AI-powered, decentralized future is not inevitable. It requires us to confront the hard, non-technical challenges of building a new system.
We must:
- Establish clear legal and liability frameworks for AI-assisted care
- Solve the complex issues of data ownership and PHI protection in a more fluid, interconnected ecosystem
- Create standardization to prevent a regulatory patchwork that stifles innovation
These are not barriers; they are essential design specifications for a trustworthy and scalable system.
The Dawn of Predictive, Ubiquitous Care
By solving these challenges, we can achieve the ultimate goal: a shift from our current reactive model to a proactive, predictive and personalized system of care. Continuous monitoring from wearables and at-home devices, analyzed by AI, can allow us to intervene before a crisis, not after. This aligns perfectly with the shift to value-based care, where incentives are based on keeping patients healthy, not just treating them when they are sick.
The heavy investments in healthcare AI from major tech players like Meta and OpenAI are a clear signal of this trajectory. They are betting on a future where AI's power in pattern recognition enables early intervention and changes the economic equation of health.
Related Article: AI's Trojan Horse: Are We Automating Medical Education or Lobotomizing It?
Final Thought
The orthodoxies of the past have given us a healthcare system that is a marvel of industrial-age thinking: centralized, siloed and profoundly inequitable. We have the opportunity, right now, to leave that obsolete model behind.
AI provides the tools to smash the silos, abolish the tyranny of geography and redesign care delivery around the patient, not the institution. This is not a technical challenge to be delegated to your CIO. It is a moral and strategic imperative for every enterprise leader. It's time to stop managing the decline of the old system and start architecting the future of health.
FAQs
Learn how you can join our contributor community.
