Key Takeaways
- AI's Dirty Secret in Medicine. It's not just writing notes; it's neurologically downgrading your doctors' ability for critical thought.
- Stop Hiring Credentials, Start Testing for Minds! That perfect diagnostic workup may be from a bot. Your hiring process must now find the real thinkers.
- The Great Medical Divide. AI is a phenomenal skills coach (for procedures) but a terrible thinking teacher (for diagnosis). Your enterprise must now manage both.
- Your Hospital Must Become a "Gym for the Mind." Don't wait for Med Schools. You must now actively rebuild the deep clinical reasoning capabilities AI is eroding.
- This Is a Patient Safety Crisis, Not an Academic Debate. The quality of your future clinical talent is being degraded right now. Leaders must act.
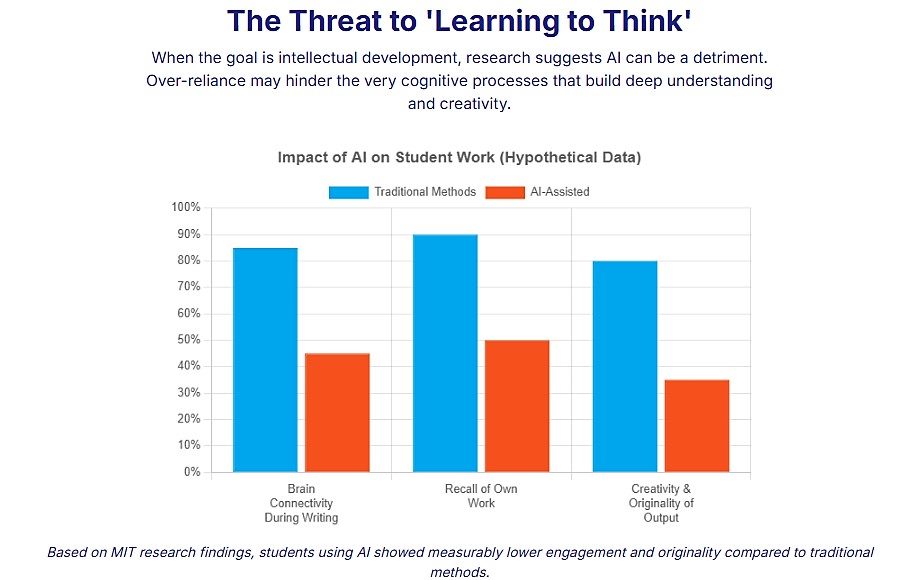
I've analyzed the data from a recent MIT study, and the neurological implications are chilling. When students use AI to do their work, their brains show measurably less connectivity. They can't recall their own arguments.
Now, imagine this isn't an English essay. Imagine it's a differential diagnosis. Imagine it's your mother's treatment plan.
We are standing on the precipice of engineering the deep, intuitive and critical thinking capabilities out of our next generation of clinicians. This is no longer an academic debate; it is an urgent patient safety crisis and a profound failure of leadership for every healthcare system, pharmaceutical company and medical technology enterprise.
The Neurological Downgrade of Medicine: AI is Hollowing Out the Minds of Your Future Clinicians
I’ve spent my career challenging the ossified orthodoxies of management, urging leaders to build organizations fit for the future. But today, I’m not just worried about the future of our companies; I’m concerned about the future of the human mind itself, particularly in the sacred domain of medicine. A revolution is upon us, and its name is artificial intelligence. But instead of heralding a new age of enlightenment, I fear we are presiding blindly over the neurological degradation of our future healers.
This isn't hyperbole. This is a data-driven alarm bell. A recent MIT study provided a stark look into the cognitive consequences of relying on AI. Students who used AI to write essays exhibited measurably less brain connectivity. Let that sink in. The very act of outsourcing the struggle of thinking, of forming an argument, left their minds less integrated, less capable of complex thought. They became strangers to their own work, unable to recall its logic.
Now, let's transpose this finding from the low-stakes world of a college composition class to the high-stakes arena of a hospital, clinic or medical facility.
Related Article: ‘AI Psychosis’ Is Real, Experts Say — and It’s Getting Worse
The Peril of the Hollowed-Out Mind in Medicine
For generations, we’ve understood that the practice of medicine is both a science and an art. The "art" is the unquantifiable magic of clinical reasoning: a doctor synthesizing a patient's story, disparate lab results, subtle physical cues and a vast repository of medical knowledge to arrive at a diagnosis. It is a process of deep, associative thinking, of seeing patterns others miss. What happens when the tool designed to assist this process instead actively degrades the underlying cognitive machinery required to perform it?
The student who can't recall their own AI-generated essay becomes the resident who can't defend the AI-suggested diagnosis. The homogeneous, less creative writing sample becomes the standardized, less imaginative treatment plan that fails to account for a patient's unique complexity. We are witnessing the rise of a generation trained to ask, as one of my students poignantly observed, "How can I get this done fastest?" rather than "What can I learn from this?" This mindset, when applied to medicine, is not just inefficient; it is existentially dangerous.
- Real-World Implication: Imagine a patient presenting with a complex set of symptoms that don't fit a standard textbook pattern. The seasoned clinician's mind roams, connecting dots from a past case, a half-remembered journal article, a subtle patient comment. This is the "associative learning" that current AI cannot replicate. The AI-reliant trainee, however, queries the system with standard inputs. The AI, finding no clear pattern in its data, returns a probable, but incorrect, diagnosis. Lacking the deeply forged neural pathways for independent critical analysis, the trainee accepts it. This is how the "art" of medicine dies, and patients along with it.
- Fact Check: The average physician must contend with a body of medical knowledge that doubles every few months. The cognitive load is immense. AI is seen as a solution, but if its implementation erodes the very reasoning skills needed to manage that load, it becomes a cure far worse than the disease.
AI as the World's Greatest Medical Skills Coach
Now, I am not a Luddite. To deny AI's incredible potential in healthcare would be foolish. While AI may be a corrosive agent to the development of deep thinking, it is a phenomenally powerful tool for learning practical skills. The potential here is breathtaking.
AI can be a tireless, infinitely patient tutor for anatomy, allowing a student to explore the human body in 3D in ways never before possible. It can create hyper-realistic simulations for learning surgical procedures, providing feedback without risking a single patient. It can drill a future pharmacist on thousands of drug interactions until the knowledge is second nature. For the "economically productive skills" side of the medical education equation — the memorization and procedural practice — AI is not a threat; it's a godsend that can democratize and accelerate learning on an unprecedented scale.
- Real-World Application: Companies are already developing AI-driven surgical simulators that provide haptic feedback and performance analytics, allowing trainees to practice complex procedures dozens of times before entering an operating room. This is a brilliant application of AI for skill acquisition, distinctly separate from the domain of diagnostic reasoning.
- Fact Check: A 2022 study in the Journal of Surgical Education and a 2025 prospective user study with medical students found that AI-driven feedback improved trainees' cognitive load and confidence. The study also found that AI-based feedback in surgical simulations improved trainee performance, highlighting its power as a skills-focused educational tool.
Related Article: From Sick Care to Smart Care: The AI Overhaul of Modern Medicine
The Leadership Mandate: Rebuilding the Clinical Mind
The crisis, then, is one of distinction and design. We have failed to separate the sacred work of forging a thinking mind from the practical task of imparting skills. As leaders of healthcare enterprises — the ultimate consumers of this educational pipeline — we can no longer be passive. We must become active architects of the future clinical mind.
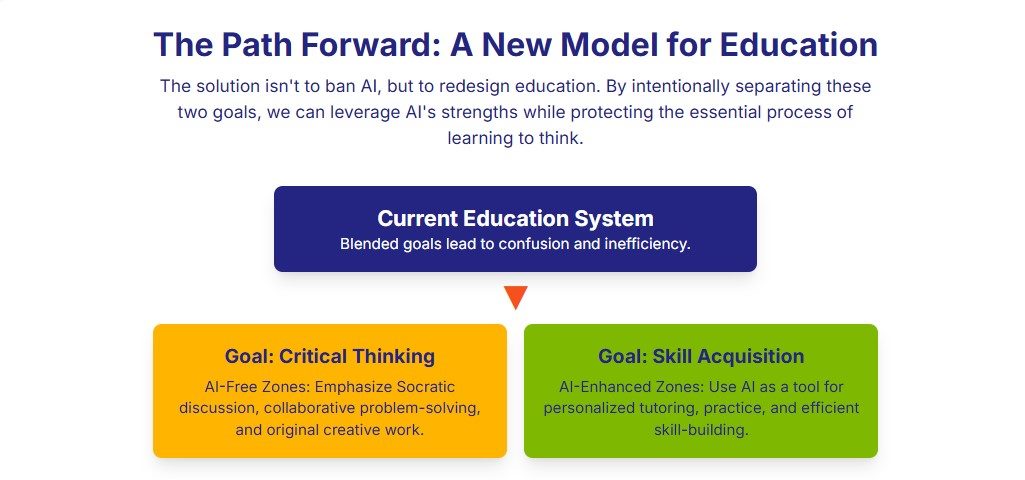
- Demand a Revolution in Medical Education: Use your influence, your residency programs, your research grants and your hiring power to demand a new standard from medical schools. They must design curricula that explicitly cultivate deep thinking, often in "AI-free" cognitive zones. Assessment must shift from information recall (a task for AI) to novel problem-solving and critical reasoning.
- Build Corporate "Cognitive Gymnasiums": Your enterprise must become a sanctuary for deep thought. Create and protect spaces for unaided human reasoning. Implement mentorship programs where senior clinicians don't just review junior doctors' work but actively deconstruct their thinking processes. Reward not just the correct answer, but the elegant, insightful and rigorous thought process that produced it.
- Hire for Thinkers, Not Just Doers: Your hiring practices are now obsolete. A flawless resume or a perfectly written case study may be the work of a clever bot. Shift to performance-based hiring that tests for real-time, unaided diagnostic reasoning. Give candidates a novel, complex case and ask them to think out loud. You are hiring a mind, not just a credential.
To Abstain or Act?
The choice is stark. Will we allow this magnificent technology to inadvertently hollow out the cognitive core of medicine, producing a generation of perfectly efficient, procedurally skilled practitioners who lack the deep, intuitive reasoning that saves lives? Or will we seize this moment of crisis as a historic opportunity to do what we should have done all along: consciously and rigorously protect and cultivate the irreplaceable art of human thinking, while using AI to master the science? The future of your enterprise, and the health of our society, depends not on the intelligence of our machines, but on our courage to defend the brilliance of our people.
FAQs
Learn how you can join our contributor community.
